M. Bhuvana Phanindra Sharma
Hall ticket no: 1701006100
A 65 year old male toddy climber by occupation came to the casualty with cheif complaints of
- fever since 3days
-abdominal distention since 2days
-urinary retention since 2days
History of presenting illness:
-Patient was apparently asymptomatic 3days back later he developed fever which was on and off, low grade type of fever, without any diurnal variation and relieved on taking medication,
-later he developed abdominal distension which was insidious in onset, gradually progressive to the current size, no aggrevating and relieving factors.
-He also complained of urinary retention since 2days associated with burning micturition .
Past history:
10 years back he had swelling and pain abdomen ;was diagnosed with left sided inginal hernia, operated , preoperative and post operative period uneventful.
4 years back patient had complaint of giddiness ; was diagnosed with Hypertension ,on medication.
6months back patient had complaint of bipedal edema ; investigations were done ct scan showed unilateral (left) stag horn renal calliculi.
1 month back he developed fever , on and off low grade type, tightness in abdomen, facial puffiness, shortness of breath, decreased appetite, pedal edema for which he was investigated and treated conservatively.
Personal history:
appetite: decreased,
Diet: mixed,
Sleep: adequate,
Bowel and blader habits: regular,
Burning micturition present,
Addictions: alcohol consumption occasionally, (one quarter a month) stopped 6 months ago.
Family history:
No significant familial history.
General examination:
Patient was conscious, coherent, cooperative. Oriented to time place and person.
Moderately built and moderately nourished.
No signs of pallor, icterus, cyanosis, clubbing, koilynchia, lymphadenopathy.
Edema - present , pitting type , grade 2
Vitals:
Temperature: 98.7°F
Pulse rate: 82bpm
Respiratory rate: 17cpm
Blood pressure: 140/70mmhg
Spo2: at room air 99%
GRBS: 134mg%
Local examination:
Abdomen
Patient was examined in supine position in a well lit room , with consent taken .
Inspection:
Shape of abdomen: distended
Umbilicus: inverted , central.
Movements of abdominal wall ,moves with respiration.
Scar of previous herina surgery seen at inginal region.
No visible pulsations , venous engorgement, sinuses.
Palpation:
Inspectory findings confirmed,
No local raise of temperature,
Tenderness -mild tenderness in suprapubic region and right hypochondrium.
Tense abdomen,
Fluid trill: not appreciated clearly
Bimanual palpation of kidney: non ballotable.
No organomegaly.
Percussion:
Normal resonant notes present over the abdomen
Liver dullness at fifth intercostal space.
Auscultation:
Normal bowel sounds were heard, no bruit present
Systemic examination:
Cvs: S1,S2 heard , apex beat- normal, no murmurs.
Respiratory system: Bilateral air entry present, normal vescular breath sounds heard.
CNS: no sensory or motor abnormalities seen, cranial nerves:normal, higher mental functions: normal, No meningeal signs , No cerebral signs.
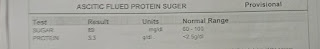
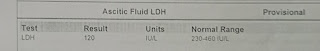
Investigations:
Provisional diagnosis:
Chronic kidney disease on Maintenance hemodialysis, with multiple renal calliculi in left kidney,With grade 4 renal pelvic dilatation.
Also a known case of hypertension since 4years.
Management:
Injection. Piptaz 2.25grs,iv,/bd
Injection. Metronidizole 0.5%gm/100ml
Tab.lasix 40mg/bd
Tab.nodosis 500mg/bd
Tab.pan 40mg/od
Tab.orofer XT /od
Tab. Shelcal 500mg/od
Tab.nicardia 20mg/bd
Syrup. aristozyme 15ml/bd.










Comments
Post a Comment