This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE HISTORY
C/O of fever since one week high grade on and off
Vomitings since 4days(5-6 episodes/day)
Nausea +
Swelling of Left Lower Limb since 4days(thigh to calf)
Pain+, local rise of temperature+
HOPI-
Patient was apparently asymptomatic one week back then had fever which is of high grade associated with chills and rigors, relieved only on medication no evening raise of temperature, no cold,cough , fever continous.
C/O vomitings since 4days - 4-6 episodes/day, content- food,non-bilious,non-projectile,no blood associated with nausea and swelling of left lower limb since 4days with pain and local rise of temperature. No C/O burning micurition, loose stools
C/O of decreased urine output
PAST HISTORY-
K/C/O DM2 since 10years(using inj. mixtard-12U-x-8U)
K/C/O HTN since 2years (using Tab. Nicardia 10mg/TID)
K/C/O CKD since 2years on conservative managment
S/P H/O Rays amputation if Right toe (great)
H/O 3 blood transfusions in February.
PERSONAL HISTORY
APPETITE NORMAL
DIET MIXED
BOWELS REGULAR
DECREASED URINE OUTPUT
SLEEP ADEQUATE
NO KNOWN ALLERGIES
NO SIGNIFICANT FAMILY HISTORY
Clinical Images-
Patient is C/C/C
BP-110/80mmHg
PR-80bpm
RR-18cpm
GRBS-111mg/do
Temperature- 100 F
Spo2-99% on Room Air
SYSTEMIC EXAMINATION
CVS- S1S2+,NO MURMURS
RS- BAE+,NVBS HEARD
P/A- SOFT,NON TENDER,BOWEL SOUNDS+
CNS- ORIENTED TO TIME,PLACE AND PERSON
INVESTIGATIONS
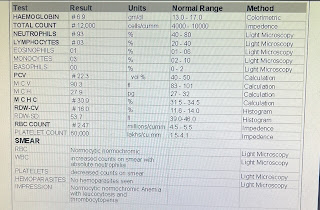
HEMOGRAM-
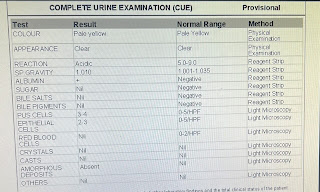
COMPLETE URINE EXAMINATION
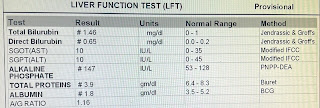
LIVER FUNCTION TEST
RENAL FUNCTION TEST
BLOOD SUGAR FASTING
SERUM IRON
ECG
Hemogram(8/5/23)(10/5/23)(12/5/23)(14/5/23)(16/5/23)(17/5/23
HB- 7.56-6.9-7.4-6.9-7.4-6.6
TLC-25,600-12,000-11,600-8,530-20,000-17,000
PLT-1,90,000-78,000-50,000-34,000-37,000-60,000
S. Creat-4.4-4.7-4.1-3.9-2.5-3.0
Urea-172-168-137-74.
PT-25secs
ONR-1.8
APTT-50secs
2D echo-
EF-48%
Trivial AR/TR/MR
Mild Global Hypokinesia, No AS/MS
Mild LV Dysfunction +, Mild LVH
Diastolic dysfunction+, NO PAH
USG findings
Grade 1 RPD changes noted in B/L kidneys
Urinary bladder shows irregular wall thickening likely cystitis
Gallbladder with Edema
Umbilical hernina omentum as content
Mild ascites.
Blood Culture(10/05/23)
No growth after 24hrs of aerobic inoculation
Culture from wound(11/05/23)
Methicillin senstive
Senstive to clindamycin, cotrimoxazle and E. Coil isolated
(Satohyloccus ) gentamycin
Urine for C/S(11/5/23)
1-2 pus cells are seen.
Klebesilla pnemonia 10*5>CFU/ml of urine isolated
Diagnosis-
Sepsis secondary to Left Lower Limb Cellulitis(resolving) with Heart Failure With Mid Range Ejection Fraction(48%)
With Acute Kidney Injury(resolving)on Chrnoic Kidney Diease With Anemia(Normocytic Normochomic) due to?CKD
With Thrmobocytopenia(resolving)with K/C/O HTN since 2yrs
S/P Rays Amputation of Great Toe( February)
S/P Fasciotomy Left Foot(13/5/23)
3 sessions of Hemodialysis were done.
TREATMENT GIVEN
1. IV Fluids NS@75ml/hr
2.Inj. Pan40mg IV/BD
3.Inj. Vitocofol 1500mg IM/BD
4.Inj. Thiamine 200mg in 100 mL NS IV/BD
5.Inj.Monocef 1gm IV/BD
6.Inj. Lasik 40 mg BD
7.Inj . HAI SC/TID acc. To GRBS
8.INj. Neomol 1gm IV/BD
9. Tab . Nodosis 500 mg PO/BD
10.Tab. Ultracet 1/2 PO/QID
11.Tab. Orofer-XT app/OD
12.Syp. Potklor PO/TID 10ml
13.Inj. Peptaz 2.25gms IV/TID
14.Inj. Clindamycin 600mg/IV/BD
15.Inj. Metrogyl 500 mg/IV/BD
16.Tab. Sporolac-DS PO/TID
17. GRBS 7. Profile Monitoring
18.2-3 Eggs whites/day
19.Strict I/O charting
20. Monitor Vitals 2nd hrly., 2PRBC transfusion was done
ADVICE AT DISCHARGE
1. Tab. AGUMENTIN 25MG PO/BD -4days
8AM- 8PM
2.Tab. CLINDAMYCIN 30MG PO/BD-4days
8AM-8PM
3.Tab. METRONODAZOLE 400MG PO/TD-4days
4.Tab. THIAMINE 200mg
5.Tab. LASIX 400 MG PO/BD-4days
8AM-8PM
6.Tab. PANTOPRAZOLE PO/BD- 4days
Before Food
7.Tab . NODOSIS 500mg PO/BD
8AM-8PM
FOLLOW UP
Review to Gen Med OPD on Monday 22/05/2023
(RFT reports)










Comments
Post a Comment