A 19yr old female SOB since 4 days primigravida with severe Anemia with left lung plueral effusion and left LL consolidation
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
19year old female came to the casuality with the
Chief complaints -
-sob since 5 days
-cough since 5 days
-fever 5 days
HOPI
Patient was apparently asymptomatic 4 months back then she developed cough (non productive) on and off, aggrevated 4 days back
C/o vomtings since 4 months (on& off)
SOB since 4-5 days( grade 2) no h/o of orthopnea,palpatations,pnd,
H/o fever 5 days back high grade and associated with chills and rigor
No h/o pain abdomen, loose stools,burning micturation,cold
Past history
Not a k/c/o HTN,DM,asthma,thyriod disorders, CAD, epilepsy,CVA
Personal history -
Diet - Mixed
Sleep - Adequate
Appetite - normal
B&B - regular
No addictions
Menstrual history -
Menarche - 13 yrs
Menstrual cycle - 5/28
LMP - 2/1/23
Gravida - 1
Family history-
No significant family history
General examination -
Patient was conscious coherent co-operative
Pallor - present
No icterus, cyanosis, clubbing, lymphadenopathy, edema.
VITALS
BP- 80/40mmhg
F/b ns@ 700ml
Bp - 90/60mmhg
PR -102 bpm
RR-22cpm
Spo2 99% at room air
Temperature -102 f
Clinical images
System examination
CVS: S1 S2 heard , jvp not raised,apex beat pounding
RS:
UPPER RESPIRATORY TRACT:
No Halitosis
No oral thrush,
No postnasal drip, pharyngeal deposits, tonsils
No sinus tenderness
LOWER RESPIRATORY TRACT:
INSPECTION:
Chest is symmetrical
Trachea – midline
No supraclavicular/infraclavicular hollowing
No Sinuses, scars, dilated veins, nodules
Movement with respiration, use of accessory muscles of respiration
PALPATION:
Trachea – midline
No Kyphoscoliosis,
No dilated veins – direction of flow, nodules
Chest movement normal
Decreased tactile vocal fremitus in left lower lobe
PERCUSSION:
Right/Left - slight dullness noted in left lower lobe
AUSCULTATION- bilateral air entry was present and decreased breath sounds in the left lower lobe ( over 8- 10 intercostal space) slight cre breath sounds
CNS: NFND
P/A: Non tender,uterus just palpated
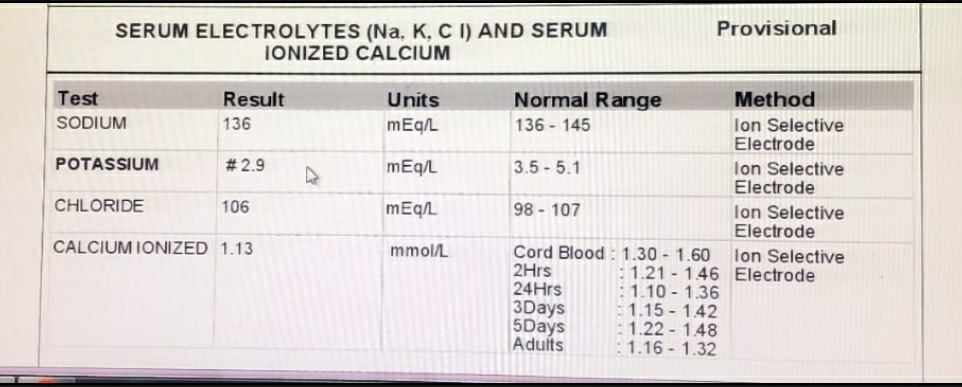
Investigations on 2/6/23
Usg on 2/6/23
Provision diagnosis -
Primi gravida with severe anemia secondary to
?Nutritional ?Hypovolemic shock with hypokalemia secondary to GI loss with left plueral effusion with left LL consolidation
Treatment history -
One unit of prbc transfusion was done
1.Iv fluids NS,Rl 50ml/hr
2.Augmentin 625 po/od
3.inj.zofer sos /iv
4.Tab. Dolo po/sos
5.inj neomol 1gm iv /sos if temp> 101.2f
6. Syp.dextromethorphan
2tsp po/TID





Comments
Post a Comment